
No. 135 (October 2020)


The APSR is committed to making sure all members are aware of opportunities — especially rewarding opportunities such as coordinating a committee by being its chairperson.
Some vacancies are coming soon and as an APSR member you are strongly encouraged to apply. However, you have only until 10 October to nominate yourself (or any other member) for the role.
Some current chairpersons will complete their two-year term at the end of November, and you have a chance to fill one of these prestigious roles from 1 December. The committees you can apply to coordinate are:
Chairing any of these committees gives brilliant opportunities for you to initiate projects and progress existing activities that contribute improvements to respiratory health.
The role also gives you a seat on the APSR Executive Committee, which enables you to influence the direction of the Society as a whole, and widens your exposure and connections with some of the most eminent respiratory physicians in the region and beyond.
Your first step is to apply!
And hurry! Only a very short time before the application deadline, 10 October.
The APSR Executive Committee is delighted to announce that Dr David CL Lam PhD, MD, FAPSR and recipient of numerous achievement awards and medals, has been selected for the position of APSR President-Elect with effect from 1 December 2020.
As advertised in earlier issues of the Bulletin, any APSR member can nominate themselves, or another member to become the APSR President-Elect, or indeed any other position, with subsequent election by voting when needed according to APSR Policy and Procedures. Leadership roles in the APSR are generally for a fixed term, and several positions will become vacant in the near future when the current holders complete their terms of office.
These opportunities for members will be advertised in this Bulletin and on the APSR website, and as an APSR member you are strongly encouraged to apply.
The APSR is committed to the highest levels of corporate governance in order to provide open, transparent and fair service to all valued APSR members, even those whose career or experience to date might not yet be as illustrious as Dr Lam's. Only then can the APSR achieve its mission to develop and sustain the highest quality of respiratory care in our region, now and in the future.

Dr Lam's involvement with the APSR stretches back to 2005, most of that time on the Education Committee which he chaired from 2011 to 2018, and the Lung Cancer Assembly where he is currently Deputy Head. He also serves on the Respirology Editorial Board as Deputy Editor while continuing his main role in the APSR as Secretary General.
In addition to his current leadership of the Hong Kong Thoracic Society (2019-2021) and earlier executive officerships on other medical associations, invited speaking engagements, and teaching appointments at the University of Hong Kong, Dr Lam continues to work as an honorary consultant at major hospitals.
His term of office as APSR President-Elect runs from 1 December 2020 until 21 November 2021, (the last day of the Kyoto Congress.)
On that day the current APSR President, Dr Yoichi Nakanishi, will hand over the presidency to Dr Lam who will then be APSR President for the next two years.
The office of the APSR President is a formidable responsibility, overseeing activities of one of the largest respiratory societies in the world, covering a geographic area which is home to half the world's population.
Therefore, please join us in congratulating Dr Lam and give him whatever is needed to support his role.

Symposium Title: Exploring The Small Airway Disease
Main speaker: Prof. Alberto Papi
St. Anna University Hospital, Ferrara, Italy
Sponsor: Orient EuroPharma


Symposium Title: Asthma Paradoxes
Main speaker: Prof. Hao-Chien Wang
National Taiwan University Hospital, Taiwan
Deputy Head of the APSR COPD Assembly
Sponsor: AstraZeneca


Symposium Title: (To be confirmed)
Main speaker: (To be confirmed)
Addendum 29 November 2020:
This AVM was held on 21 November 2020 with the title Achieving Better Diagnoses and Outcomes for Patients with Respiratory Infections, With or Without a Pandemic. The main speaker was Dr Tufik Assad
Sponsor: BioMérieux and BioFire

For each Symposium, authors of the best three abstracts will be invited to present at the Assembly Virtual Meeting. Their abstracts will also be published in a special Assembly Virtual Meeting Respirology Supplement.
For the latest news, see apsr.info



The Bronchoscopy and Interventional Techniques Assembly understands that our members have been heavily involved with COVID-19 management and guidelines in 2020. We do hope that everyone has remained safe and we look forward to the day when we can meet face to face again at a future congress – hopefully in Kyoto 2021!
Many of our members will already be aware that Respirology has recently published a special edition: Interventional Pulmonology Pearls, which contains a series of reviews from experts around the world and the Asia-Pacific region. We encourage our members to take advantage of this excellent review series which provides an update on many bronchoscopic and interventional techniques relevant to many centres' practice.
For now may we stay in touch "virtually" and continue to improve the field of interventional pulmonology research and innovation.
Dr Phan Nguyen
Head-Elect of the APSR Bronchoscopy and Interventional Techniques Assembly



Peacock et al. recently published a paper involving idiopathic pulmonary arterial hypertension (IPAH) and co-existing lung disease, as defined by the FEV1, FVC, TLC, %pred ≥60%, and lung findings on CT (Pulmonary Circulation 2020; 10(1) 1–8).
The patients were older, predominantly male, more likely to be current or ex-smokers, and had a lower DLCO. They showed improved 6-minute walk distance after PAH-targeted therapy, but poor survival compared to patients with IPAH and no lung disease; however, the severity of lung disease on CT was not mentioned. When we focus on PH due to respiratory disease (Group 3 PH), even patients with severe lung disease on CT may have mild ventilatory impairment.
Combined pulmonary fibrosis and emphysema is well-known to be associated with mild ventilatory impairment and low DLCO, concomitant PH, and poor survival. Such patients are more likely to be included in Group 1 (IPAH and co-existing lung disease), but they should be included in Group 3 PH.
We should focus on imaging analysis for Group 3 PH and quantifying the severity of lung disease on CT is needed. Combined imaging and respiratory functional analysis by respirologists or radiologists could facilitate the accurate differentiation of Group 3 PH from patients with PAH and co-existing lung disease.
Please join our assembly for further research.
As you might know, the APSR is developing a library of respiratory cases to be used for education and training of APSR members; please see the example below. The APSR Assembly kindly invites its members to submit cases for this library online. Please see apsresp.org/education/teaching-library/index.php.
Thank you for your kind consideration and we are looking forward to seeing you at the next meeting in Kyoto.
Dr Nobuhiro Tanabe, Assembly Head
Dr Masayuki Hanaoka, Assembly Head-Elect
Dr Talant Sooronbaev, Assembly Deputy Head



The Respiratory Neurobiology and Sleep Assembly is planning to issue a position statement regarding either the standard diagnostic process or the treatment strategy for the sleep apnoea syndrome.
We strongly feel that we should take into account regional and local circumstances in establishing these issues, and call for ideas, suggestions and questions from the assembly members.
We are also looking for corresponding author(s). The roles of the corresponding author(s) are to write, edit and revise the position statement as a member of a post hoc committee with the Respiratory Neurobiology and Sleep Assembly leaders, taking primary responsibility for communication with the APSR official journal Respirology.
Dr Yoshitaka Oku, Assembly Head
Dr Ning-Hung Chen, Assembly Head-Elect
Dr Hiromasa Ogawa, Assembly Deputy Head
To accept the invitation to be involved or for further information, please contact APSRinfo@theapsr.org

Keystone Symposia is offering a limited number of free registrations to researchers from low- and middle- income countries (LMICs) to participate in our new eSymposia series. This new digital format enables the inclusion of more diverse voices and global perspectives in conversations at the forefront of science and medicine, which are essential to shape research that serves the broad needs of all of humanity.
Award recipients will be provided with unique career-advancement opportunities, including:
Applications are currently being accepted for all eSymposia through January 2021, and are open to LMIC scientists and clinicians of all career stages including students, post-docs, fellows, professors, doctors, etc.) working in relevant fields of interest. Please help spread the word to your colleagues!
Keystone Symposia events list keystonesymposia.org/KS/Online/Events/All_Events.aspx
Keystone Symposia financial aid details keystonesymposia.org/KS/Online/Financial_Aid/Financial-Aid-Landing.aspx
See a collection of COVID-19 material on the dedicated COVID-19 page on the APSR website.
Respirology Case Reports, Volume 08 Issue 7
The spotlight this month is on
Each month we share details of activities of a particular country, region or society.
If you would like the spotlight to be on your country, region or society next month, contact the Bulletin Coordinator or APSR Secretariat.
Two articles kindly provided this month by Dr Dushantha Madegedara, Head of the Clinical Respiratory Medicine Assembly: the COVID-19: Sri Lankan Experience, followed by Trends of Respiratory Diseases in Sri Lanka; A Tale of Two Decades
Madegedara RMD1, Karunadhipathi UN1, Yasaratne BMGD2
1Respiratory Medicine Unit-2, National Hospital, Kandy, Sri Lanka
2Department of Medicine, Faculty of Medicine, University of Peradeniya, Sri Lanka
COVID-19 pandemic is an unprecedented global health crisis, ravaging human population in 2020. It is primarily transmitted between people via respiratory droplets and person-to-person contact routes. Sri Lanka, an Island country lying in the Indian Ocean, was also affected with this newly discovered virus.
[ Click any image to enlarge ]
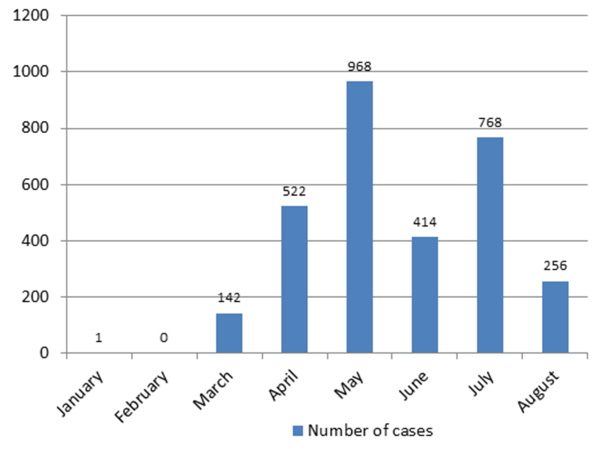
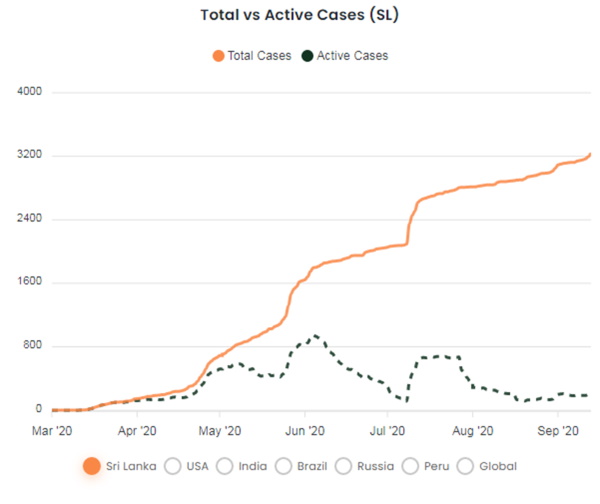
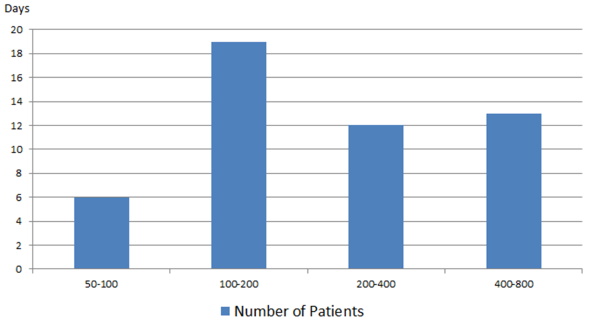
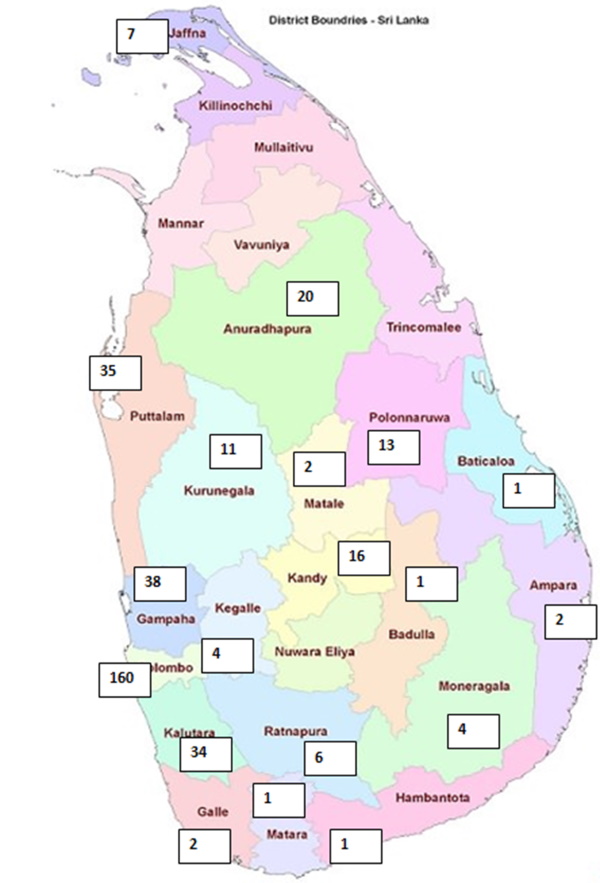
The first case of the virus was confirmed in Sri Lanka on 27 January 2020, after a 44-year-old Chinese woman from Hubei Province in China was admitted to the National Institute of Infection Diseases. By the time this report was prepared – 13 September 2020 - a total of 3,195 confirmed cases, 2,996 recoveries, and 12 deaths had been reported in the country. Sri Lanka has thus far been successful in containing the disease and opening up the country back to a near normal functional state. It would be useful to revisit the methods used to achieve such disease control by a country with limited health resources, and to discuss any factors that may have contributed.
Following the detection of first case in late January, the second patient, a native with foreign contact, was diagnosed in early March. By the time the total number of confirmed cases reached 87, the Sri Lankan government announced a lockdown style curfew in the country on 25 March 2020. This helped to maintain the outbreak under epidemiological stage II for the next four weeks.
A collaborative COVID-19 Operational Body was formed on 23rd March with officials from Government, Health Ministry and Armed Forces. National guideline committees, Provincial and District operational committees, Hospital COVID cells were formed representing all parts of the Island. COVID treatment centres were developed in infectious disease hospitals and other selected hospitals, while isolation facilities were established in all hospitals. Public health teams were reinforced with coordinating bodies and community based quarantine centres were established. Laboratory facilities were expanded in major microbiological centres.
The first confirmed COVID death in the country occurred on 29 March. The diagnosed cases in this period were mainly from foreign contacts and their close associates, making it practical for health officials to carry out an effective quarantine process. On 23 April, 38 persons confirmed COVID and of them 30 were from officers of the Welisara Navy Camp involved in moving a group of drug addicts who tested positive for the coronavirus to quarantine. Later on, this proved to be a major step in the outbreak, spreading to 950 navy officers and close contacts to date.
With a large number of cases getting detected among overseas returnees and COVID pandemic becoming uncontainable in many parts of the world, the Sri Lankan Government decided to follow suit in closing its international airports for routine passengers from 1 May. However, Sri Lankan citizens stranded in many parts of the world were given necessary support and return air travel through respective embassies.
the Sri Lankan Government announced lifting the curfew after six weeks on 11 May, except in selected high risk areas, meaning that the public could start going to workplaces by maintaining social distancing and protective measures. However schools and universities were still closed and public gatherings, festivals, celebrations were banned. By that time total number of confirmed cases was 863, total number recovered 343 and total number of deaths 9.
To date, Sri Lanka has diagnosed 3,195 confirmed COVID-19 cases. Of those, 1,235 were Sri Lankan returnees from other countries, 950 were from the Sri Lanka Navy and their close contact clusters, 650 from Kandakadu quarantine center cluster and 47 were foreign travellers. All Government and private institutions are open and functional, with people adhering to health control guidelines, and schools and universities are open. Airports are still closed for routine passengers considering the global status of the pandemic.
In conclusion, Sri Lanka, despite being a country with limited health resources, has thus far been successful in containing the COVID-19 pandemic and reopening the country back to a near normal state. This achievement is largely due to well-coordinated and efficient public health activities including prompt diagnosis, contact tracing, effective quarantine processes, public education and preventive strategies. Being an island nation with a tropical climate, having a bearable population density, and access to various western and native treatment options, may have helped the Sri Lankan community in this cause. COVID-19 has tested the ability of all sectors in the country to mount a swift response to a pandemic situation. Continuous vigilance and preparedness will be required for coming months to years for a sustainable effort.
References
Madegedara RMD1, Karunadhipathi UN1, Yasaratne BMGD2
1Respiratory Medicine Unit-2, National Hospital, Kandy, Sri Lanka
2Department of Medicine, Faculty of Medicine, University of Peradeniya, Sri Lanka
Sri Lanka, an island country officially known as the Democratic Socialist Republic of Sri Lanka is situated off the southern coast of India in the Northern Indian Ocean of South Asia, separated from the Indian sub-continent by a natural bridge of shallow water, known as Palk Strait.
The nation has a total area of 65,610 square kilometres, including 2,905 square kilometres of inland water. Sri Lanka’s climate is tropical, consists of wet and dry seasons and it is affected by its proximity to the equator as well as the elevation above sea level and the monsoons. The mean temperature ranges from 26.50° C to 28.50° C (79.70° F to 83.30° F) in the coastal area and from 14° C to 24° C (58° F to 75° F) in the upland area.
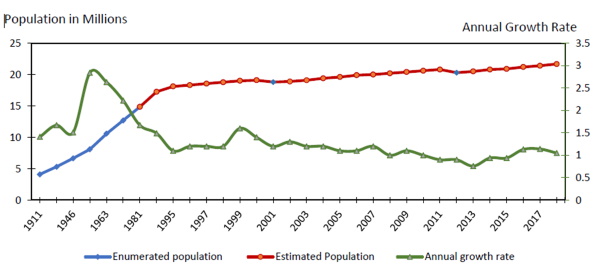
The fourteenth national Census of Population and Housing (CPH) in 2012 enumerated that the population was 20,359,439. Annual growth rate has been a steady 1.0% - 1.5% for last several decades (Figure 1).
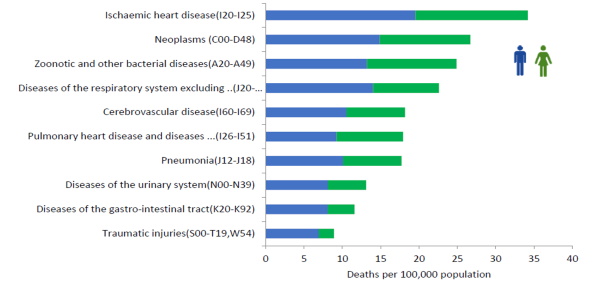
During last many decades, the Crude Death Rate (CDR) of Sri Lanka has been steady, with 6.4 deaths per 1,000 population in 2017 (Figure 2). However the Crude Birth Rate (CBR) has been steadily declining, which has led to doubling the percentage of elderly population from 6.6% to 12.4% during the period 1981-2018.1
[ Click any image to enlarge ]
Traumatic injuries were major cause of hospitalization in 2018. Diseases of the respiratory system excluding diseases of upper respiratory tract, pneumonia and influenza, are the third leading cause since 2009 up to 2018, except in the Year 2017, when it was ranked as the fourth leading cause (Figure 3).2
Diseases of the respiratory system excluding diseases of upper respiratory tract, pneumonia and influenza were the third leading cause and pneumonia was the seventh leading cause of hospital deaths in 2018 (Figure 4).

Obstructive airway diseases comprise a major proportion of lung diseases in all age groups in the country, carrying a large disease burden. The Sri Lankan arm of the International Study of Asthma and Allergy in Children (ISAAC) done in 2002, has revealed the presence of persistent nocturnal cough or wheezing among preschool and school children to be over 20%.3
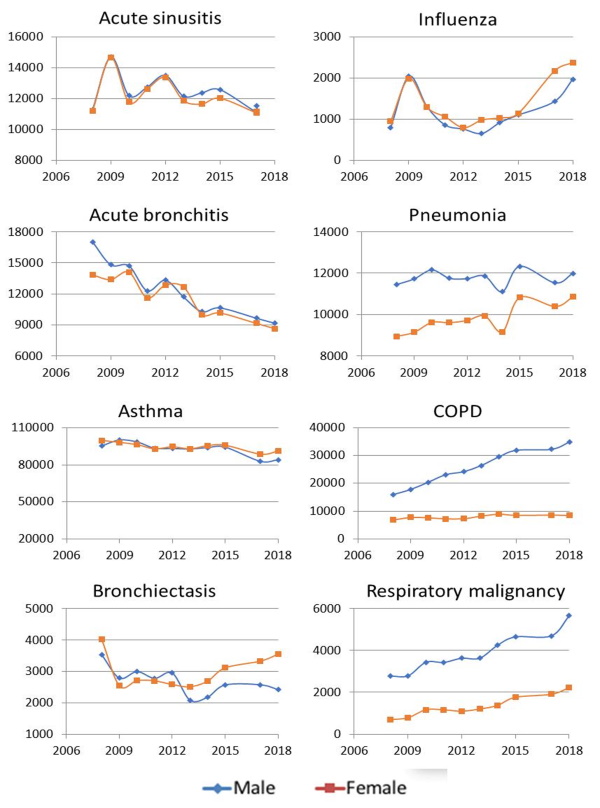
Trends of some common respiratory diseases in Sri Lanka during the last two decades, based on hospital live discharge statistics, are shown in Figure 5. Acute sinusitis, influenza, acute bronchitis, asthma and bronchiectasis show similar trends in both males and females. However, a male preponderance has been observed in pneumonia, COPD and respiratory malignancies, likely owing to the cultural fact that cigarette smoking is almost negligible in a traditional Sri Lankan female.
Viral respiratory infections including acute sinusitis and bronchitis are very common in the country throughout the year. A slight decreasing trend of hospital cases of these two diseases has been observed both in males and females since 2006. However, it is important to remember that most with such illnesses would not get admitted to hospitals. Conversely, a steady rise of pneumonia cases was noted both in males and females.
Seasonal Influenza has been generally observed during April to June and again in November to January in Sri Lanka. Globally seasonal influenza has shown a decreasing trend according to the World Health Organization surveillance data (2015). ).4 When looking at the trend of Influenza in Sri Lanka, after an initial drop in case numbers in 2013, there has been a steady rise.
The highest numbers of cases were noted for asthma and COPD. Throughout the last decade the number of hospital cases of asthma in both males and females has been somewhat steady. The Burden of Lung Diseases (BOLD) survey revealed an overall 10.5% (95% CI: 8.8–12.2%) prevalence of COPD among Sri Lankan adults aged over 40 years.5 Among males, the prevalence was 16.4% (95% CI: 13.2–19.5%) compared to 6.0% (95% CI: 4.2%–7.7%) in females who are largely nonsmokers. The available latest statistics revealed gradual increment in number of hospital cases with significant male predominance. Among the male population the number of hospital cases has doubled during period from 2008-2018.
The trend of bronchiectasis in Sri Lanka has been fluctuating over the period from 2008 to 2018. Reported cases of lung malignancies has been increasing and there is a significant male predominance.
The island-wide preventive and curative services of the National Programme for Tuberculosis Control and Chest Diseases (NPTCCD) in Sri Lanka have been successful in maintaining the intermediate burden state of TB in the country. Universal TB treatment coverage is 64% and incidence of multidrug resistance remains below 0.03 per 1000 individuals. Nevertheless, despite wide public awareness campaigns around the year, the national case detection rate of TB remains below the WHO estimates, which is a public health concern).6
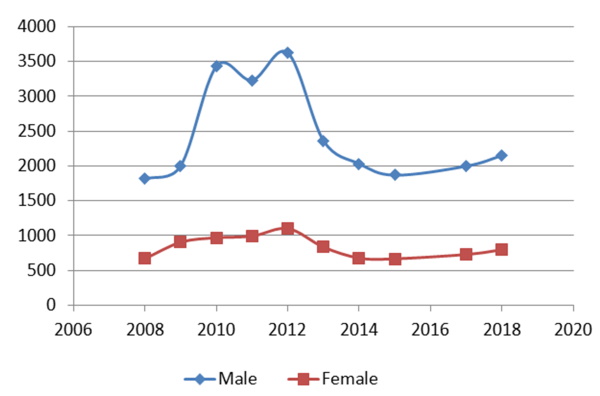
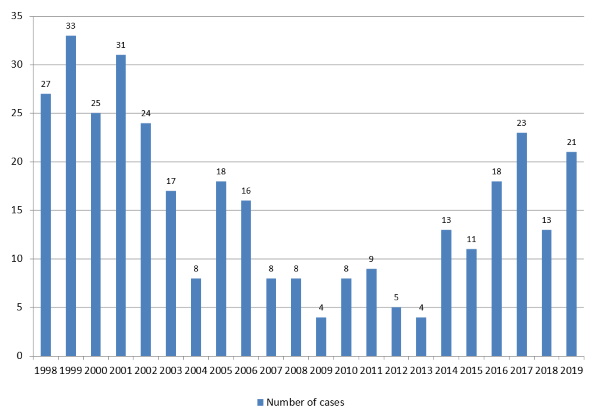
In Sri Lanka, annually over 8000 cases of tuberculosis are detected. Microbiologically confirmed pulmonary tuberculosis comprises a major fraction of it, where there is a significant male preponderance (Figure 6). The number of cases has been steady from 2013 to date.
Clinically diagnosed pulmonary tuberculosis (smear negative) cases were also noted to have a steady course throughout this period (Figure 7). This number is expected to decline with the widespread availability of nucleic acid amplification testing (XpertMTB) in all districts. Numbers of miliary tuberculosis cases are comparatively much less and remain static (Figure 8).

Sri Lanka has been successful in keeping the incidence of multi-drug resistant tuberculosis (MDR-TB) under control, mainly by strict follow-up of patients on anti-TB treatment (ATT) in the community and regulating prescriptions of ATT (Figure 9). Community acquired primary MDR-TB is negligible.
Being a tropical country with a frequently fluctuating climate, acute and chronic respiratory diseases are a heavy burden to Sri Lanka. Diseases of the respiratory system, excluding diseases of upper respiratory tract, pneumonia and influenza, have remained the third leading cause of hospital admission since 2009. Highest cases were noted for bronchial asthma, in which hospital admissions have been static over the last decade. However, COPD and lung cancer admissions are on the rise, with a noteworthy male preponderance, likely owing to late effects of male smoking and other environmental factors. The island maintains the intermediate burden disease state of tuberculosis, with a very low incidence of drug resistance, while being in the South Asian region with a high tuberculosis burden.
References
The KATRD International Conference 2020 will be held virtually on 12-13 November 2020.
As the global impact of the coronavirus pandemic grows daily, the priority is always the health and safety of our community and participants.
The KATRD has developed into an international academic conference thanks to your efforts and support. Last year, the conference attracted 1,067 participants from 20 countries. The KATRD will build a dynamic, interactive, and inclusive virtual conference.
Internationally renowned speakers will be in attendance to discuss the latest trends with plenary sessions and symposiums which will cover all areas of our rapidly changing medical environment. Throughout these programmes, the Conference will offer exciting opportunities to gain insights and new ideas as you are connected to globally well-known speakers and enthusiastic fellow scholars. This Conference hopes to build an international network and promote collaboration.
The registration fee has been substantially reduced to encourage students and trainees from non-presenting attendees from all over the world to attend the conference on a new digital meeting platform.
| Registration fee | |||
| Early (until 16 October) | Late (after 16 October) | ||
| Medical Doctor, Professor | Domestic | KR₩ 20,000 | KR₩ 50,000 |
| Overseas | US$ 20 | US$ 50 | |
| Fellow, Resident, Nurse, Military Doctor, Researcher, etc. | Domestic | KR₩ 10,000 | KR₩ 30,000 |
| Overseas | US$ 10 | US$ 30 | |
Registration will provide each participant with an access code to participate in sessions.
The conference has an impressive line-up of invited international speakers.




Several other eminent APSR members will be presenting important topics during the Conference. See the speaker list and full programme at katrdic.org/program/sub02.php
The PCCP celebrated World Lung Day by paying tribute to the modern heroes. Advocates of protecting the environment and making efforts to save our surroundings — Advocates of clean air for human health.
(You might need to zoom your screen to fully enjoy their video.)
Also due to the pandemic, the date of the World Conference on Lung Cancer has changed.
This had been scheduled to be held on 9-12 August 2020 and has been postponed to 26-29 January 2021.
Please check the IASLC website wclc2020.iaslc.org for the latest details.
MANILA (Reuters) 14 September 2020 - Experts described as dangerous and premature on Monday the Philippines' decision to cut the social distancing minimum to 30 centimetres (12 inches) on public transport, as the country saw another daily record in newly confirmed COVID-19 deaths.
Reducing gaps between passengers incrementally to a third of the 1 metre minimum could backfire, experts and medical professionals warned, and prolong a first wave of infections that the Philippines has been battling since March.
The new rules took effect on Monday [14 September], when the country reported 259 new confirmed deaths, a record for the second time in three days. Total fatalities increased to 4,630, while infections have doubled in the past 35 days to 265,888, Southeast Asia's highest number.
"This will be risky, reckless and counter-intuitive and will delay the flattening of the curve," Anthony Leachon, ex-president of the Philippine College of Physicians, told news channel ANC. "Even if you wear a face shield and mask, reducing the distance between, it will be dangerous," he said, adding that 1 or 2 metres was the minimum international standard.
The transport ministry's new rules cut the distance to 75 cm on Monday [14 September], 50 cm on 28 September and 30 cm on 12 October. Conversation and phone calls are now prohibited.
The health ministry on Monday urged the public to be "extra vigilant" in tight travel conditions and to choose other transport modes if possible. Manila's transport systems are notoriously crowded, with commutes typically involving long queues and several changes.
"It is likely that we will see an increase in cases and our recovery will slow if we do this now," said epidemiologist Antonio Dans. Dans is a member of a health professionals alliance that last month pleaded for a tightening of Manila's lockdown - a "timeout" to stop hospitals being overrun. It urged a rethink of the 30 cm rule.
The plan aims to help an economy that the government sees contracting 5.5% this year, the worst shrinkage in 35 years. "Reopening the economy will never happen unless the viral transmission is controlled," added Leachon, a former advisor to the government's COVID-19 task force.
Singapore has started distributing Bluetooth contact-tracing tokens to its five million residents to help contain the spread of Covid-19.
The tokens, which can be worn on a lanyard or carried, are a hardware version of its existing contact-tracing app which was rolled out in March. Like the app, they use Bluetooth to look for other users' devices and then log any contact with those devices. They could be popular with older people who do not use smart phones.
The government also hopes the tokens will help to further reopen the economy, by enabling conferences to restart and providing better tracing in higher risk settings, such as busy hotels, cinemas and gyms.
The initial rollout is happening in areas with a greater concentration of elderly people, who are both at a greater health risk from Covid-19 and less likely to own a smart phone. But the token will be available to all citizens, including foreign residents.
Singapore residents currently check-in to shops and office buildings using a separate SafeEntry system, that makes use of QR codes to log users' presence. For some higher-risk activities, SafeEntry will now also require the app or token to check in.
Better for privacy?
A consultant tapped by the government's technology agency to provide feedback on the token said it's a better option for anyone concerned about privacy. "I would prefer to use the token over the app," said Bunnie Huang, who lined up for a token on the first day it was available.
Like app, information is stored on the token, purged regularly and is only uploaded - or in the case of the token physically handed over - to the Ministry of Health if the user tests positive.
The advantage to a hardware-only version, said Mr Huang, is that it makes it impossible for a software update to surreptitiously turn on location data or other sensors without the user noticing. "With the token, if I want it off, I know how to destroy it," he said.
The token will also help to cover people without a smart phone, and those who have encountered functionality problems with the app, he said.
Singapore was the first government to introduce a contact tracing app nationally in March. Since then, about 2.4 million people have downloaded the app, with about 1.4 million using it in August.
Singapore government figures have long acknowledged that those numbers need to increase to make the app and the token effective. But the Ministry of Health said the program has helped to reduce the time it takes to identify and quarantine close contacts of Covid-19 cases from four days to two.
The city-state has been more enthusiastic about contact tracing apps than many other countries, which have been slower to introduce apps or have struggled to make good use of them.
Extracted from BBC News 15 September 2020
bbc.com/news/business-54143015

The Teaching Library is open for your self-study. Challenging yourself to choose the correct procedure for any of the cases in the Library at apsresp.org/education/teaching-library/index.php.
Many more cases are needed for this Library and any member is welcome to submit a case (or cases!) through the same link as above.
The following article has recently been selected from Respirology for its specific educational value. Previous articles on further topics can be seen at apsresp.org/education/articles/index.html
Of special interest to those working in:
* Asthma
* Respiratory structure & function
* Immunology
* Clinical Respiratory Medicine
Acute effects of e-cigarette vaping on pulmonary function and airway inflammation in healthy individuals and in patients with asthma Serafeim-Chrysovalantis Kotoulas, Athanasia Pataka, Kalliopi Domvri, Dionisios Spyratos, Paraskevi Katsaounou, Konstantinos Porpodis, Evangelia Fouka, Aikaterini Markopoulou, Katalin Passa-Fekete, Ioanna Grigoriou, Theodoros Kontakiotis, Paraskevi Argyropoulou and Despoina Papakosta
onlinelibrary.wiley.com/doi/10.1111/resp.13806/full (October 2020)
Comment by Dr Mark Lavercombe:
The rapid escalation in 'vaping' using electronic nicotine delivery devices has not yet been matched by data demonstrating their safety. In a cohort of asthmatic patients taking regular inhaled corticosteroids, acute markers of airway inflammation and pulmonary function changed within five minutes of e-cigarette vaping and this did not occur in healthy controls. The authors discuss the implications for future research in both healthy subjects and patients with pre-existing obstructive lung diseases.

Dr Petru Emil Muntean FAPSR (Pitesti Queen Mary Hospital and Arges Emergency County Hospital, Romania) has kindly sent his donation towards the Society's goals, as outlined at apsresp.org/members/donors.php.
The APSR is profoundly grateful for his generosity.
Congratulations to Dr Fukuda (University of the Ryukyus, Japan) an APSR Young Investigator awardee at the virtual ERS International Congress 2020.
Here is his report:

I'm greatly honoured to receive the Young Investigator Award at the virtual ERS International Congress 2020. I'd like to express my deep gratitude for the numerous supports from ERS and APSR.
I was very pleased to have the opportunity to present our work entitled "Time to advanced airway management and neurologically favourable survival after out-of-hospital cardiac arrest" in the Oral Presentation Session. In the presentation, I showed the findings of our nationwide population-based observational study of out-of-hospital cardiac arrest from 2014 to 2017, that delay in advanced airway management was associated with decreased chance of neurologically intact survival after out-of-hospital cardiac arrest. Thanks to heated discussion and constructive comments, the session was very exciting and beneficial for me. This virtual live session was my first experience, so I was very nervous before the start of the session, but it was fun and exciting actually.
During the congress, I got the latest updates on state-of-the-art Critical Care Medicine, and valuable take-home knowledge from cutting-edge presentations of original scientific research in several sessions. Also, I could view numerous interesting e-posters in a variety of presentations, including the COVID-19 sessions. The latest findings from top clinicians and scientists around the world will be of great help to me.
Thank you again for the support from the APSR and ERS to attend the virtual ERS International Congress.
Congratulations to Dr Lin (Department of Internal Medicine, National Taiwan University Hospital) an APSR Young Investigator awardee at the virtual ERS International Congress 2020.
Here is his report:

It was a great honour to attend the virtual congress of ERS 2020 representing Taiwan and the National Taiwan University Hospital. This was a special year due to the global pandemics and health care personnel worldwide were facing enormous challenges in patient care and disease control. Thanks to the internet, we were still able to communicate with each other and still able to have an international conference in a virtual form.
During the presentation session, I was able to meet other excellent doctors and scholars working on respiratory medicine and had some very good times exchanging experiences. It was a unique and pleasant experience during the whole ERS meeting.
I had the opportunity to present the research entitled "Higher adverse drug reactions but better completion rate of twelve-dose weekly rifapentine plus isoniazid comparing with nine-month daily isoniazid for latent tuberculosis infection among patients under maintenance dialysis", which has nothing to do with COVID-19. This study addressed the issue of regimen selection in patients under hemodialysis when treating latent tuberculosis infection.
The online oral presentation proceeded as planned smoothly and we had a great discussion session regarding several critical and meaningful questions for the study both with the chairs and the audience. While we ended the sessions with more than 700 people viewing, unfortunately the experience was still not as interesting as a real-life presentation and face to face interaction.
Again, with greatest and sincerest gratitude to the APSR and ERS for giving me the credit on the research. I look forward to future chances of (face to face) meeting and sharing each other's work again in the near future!
Congratulations to the following members who have recently become Fellows of the APSR:
A warm welcome to the following members who have recently joined or re-joined APSR assemblies.
| Digambar Behera | Clinical Respiratory Medicine Tuberculosis Lung Cancer |
| Chee Shee Chai | COPD Asthma Respiratory Neurobiology and Sleep |
| Muhammad Imran | Clinical Respiratory Medicine Clinical Allergy & Immunology Respiratory Infections (non-tuberculous) |
| Arnaud Prigent | Clinical Respiratory Medicine COPD Critical Care Medicine |
| Chandan Kumar Sheet Chandan Kumar Shit | Bronchoscopy and Interventional Techniques Critical Care Medicine Interstitial Lung Disease |
| Ying Tianlei | Respiratory Infections (non-tuberculous) Lung Cancer COPD |
Here are the main respiratory events in Asia-Pacific region for the next few months. You can see our full listing on the APSR Calendar.
For more pulmonology events, see apsresp.org/calendar.html
(These events are for information only and APSR endorsement should not be assumed.)
If you have news of interest to APSR members, please send details to one of the Bulletin Coordinators: Prof. A Azuma (a-azuma@nms.ac.jp) or Prof. C K Rhee (chinkook77@gmail.com).